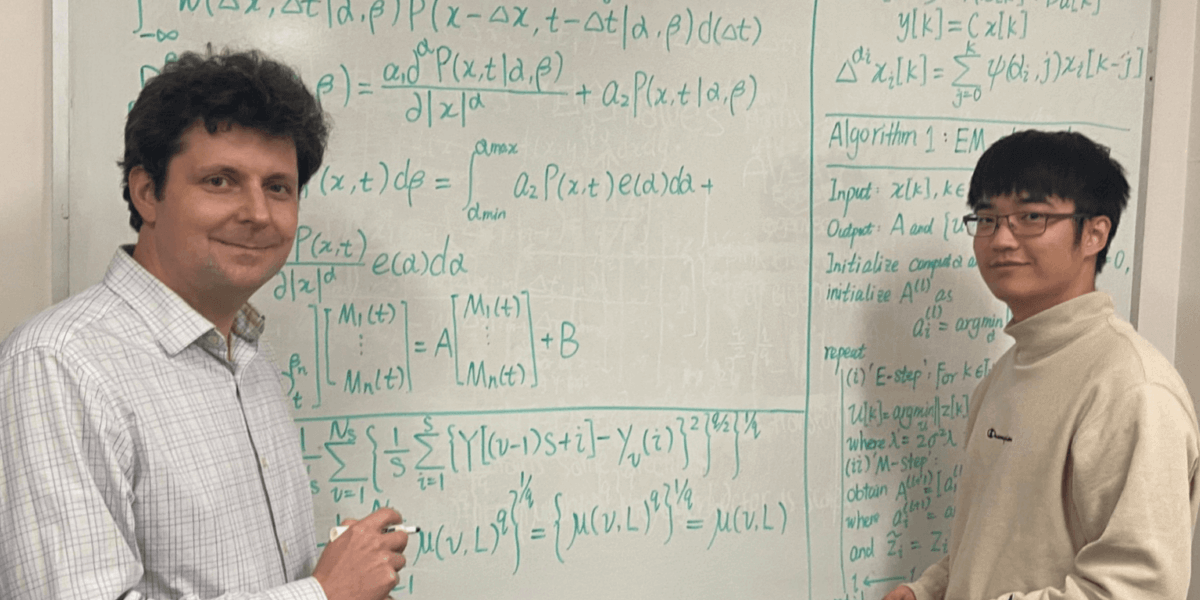
Paul Bogdan and Chenzhong Yin with a summary of their research (Photo/Courtesy of Paul Bogdan)
Chronic obstructive pulmonary disease, or COPD, is a chronic inflammatory lung disease that causes obstructed airflow from the lungs. It is the third leading cause of death worldwide, according to the World Health Organization, with more than 150,000 Americans dying from it annually.
So, when USC Viterbi’s Paul Bogdan and his research team received a set of data illustrating a surprisingly low accuracy rate of COPD diagnoses, they decided to combine the novelty of data geometry, machine learning and the subtleties of a COPD diagnosis to develop a more reliable and accessible method of detecting COPD.
Currently, doctors use the spirometry test to measure how much air a patient can breathe out in one continuous breath to monitor lung strength. However, that method is subject to varying interpretations: two doctors could come to different conclusions using the same results from a spirometry test, Bogdan said.
Not to mention, the spirometry test is sometimes unreliable. That’s because it relies on the patients’ voluntarily breathing into the tube, which, Bogdan said, may not always accurately reflect the health of their lungs. For instance, smokers might blow extra hard into the device to fool the spirometer into thinking they have strong lungs.
“It’s very much like when the dentist asks, ‘Are you flossing?’ And the patient will say, ‘Yes, of course.’ Even when they have not been,” said Bogdan, the Jack Munushian Early Career Chair and associate professor of electrical and computer engineering.
The New Model
To help achieve more accurate diagnoses, Bogdan’s research team has harnessed the power of artificial intelligence (AI). They have shared their recent findings in the research paper entitled “Fractional Dynamics Foster Deep Learning of COPD Stage Prediction” that appeared in February in the prestigious “Advanced Science” journal.
Bogdan’s team created an AI system that people can’t trick. Patients wear a small patch on their arm embedded with a sensor. While the doctor completes the normal physiological exam on the patient, the device monitors 12 signal records such as the respiratory inductance plethysmography (RIP), which signals breathing efforts, and the wireless pulse-oximeter, which signals oxygen saturation levels.
“In under one minute,” Bogdan said, “the device can determine a diagnosis with 98.5% accuracy.”
In addition to this increased accuracy, this new device makes COPD diagnosis and monitoring easier. In the long run, this device would not even need a doctor’s supervision. Rather, it could record data passively to cell phones and securely share it with hospitals. This way, even patients without direct access to physicians from remote areas could have their health monitored and even receive an early-stage diagnosis – the key to preventing the onset of later, more serious COPD.
“Our model is very inexpensive compared to traditional medical models,” said Chenzhong Yin, a third-year Ph.D. student at the Ming Hsieh Department of Electrical and Computer Engineering who worked on Bogdan’s NSF-funded cyber-physical systems research project. “For the traditional approach, a lot of money is spent to train doctors and visit them for exams, but our model can just analyze signals passively and make predictions for various COPD stages.”
The Team’s Philosophy
To analyze long-time-series-data, Bogdan’s team used a fractional dynamic mathematical model they have pioneered to detect different stages of COPD—from stage 0 (healthy) to stage 4 (severe). This involved measuring the fractal memory and coupling among physiological signals—in healthy people, physiological signals would have both short- and long-range memory, while unhealthy people presented memory in a narrower range.
Bogdan said his research team is one of the first to apply the meaning of these mathematical structures and fractional derivates to medical diagnosis processes.
Previously, his team conducted research on diabetes, developing a cost-effective method to capture the complex dynamics of blood glucose in diabetes patients using a fractal calculus concept.
“We do not like to rely on existing mathematical models,” Bogdan said. “We like to look at the biological system and its available data and study it the same way Newton studied gravitation: looking at the data and asking questions that nobody asked before.”
Perhaps the most interesting part of this research is its minimal cost and small size of the architecture. While traditional machine learning models would take millions of data samples of many different signals, Bogdan’s method reduces the focus to just a few physiological signals key to determining the onset of COPD in patients.
“So then, the size of the machine learning is really just that of a small class project,” Bogdan said. This efficiency raises hopes for the model to be replicated for other medical diagnoses in the future.
Bogdan’s team has been working with Stefan Mihaicuta, a medical expert on COPD and a professor at the University of Medicine and Pharmacy of Timisoara in Romania, to discuss and analyze their predictions. Mihaicuta also helped develop a comprehensive and unbiased set of medical data for the model to avoid repeating the mistakes of the spirometry test.
“We want to make sure that it all makes sense for a physician. We don’t just do mathematics for the sake of doing mathematics,” Bogdan said.
His team plans on presenting this work at the European Respiratory Society, Congress in Italy this September.
Published on April 13th, 2023
Last updated on April 13th, 2023