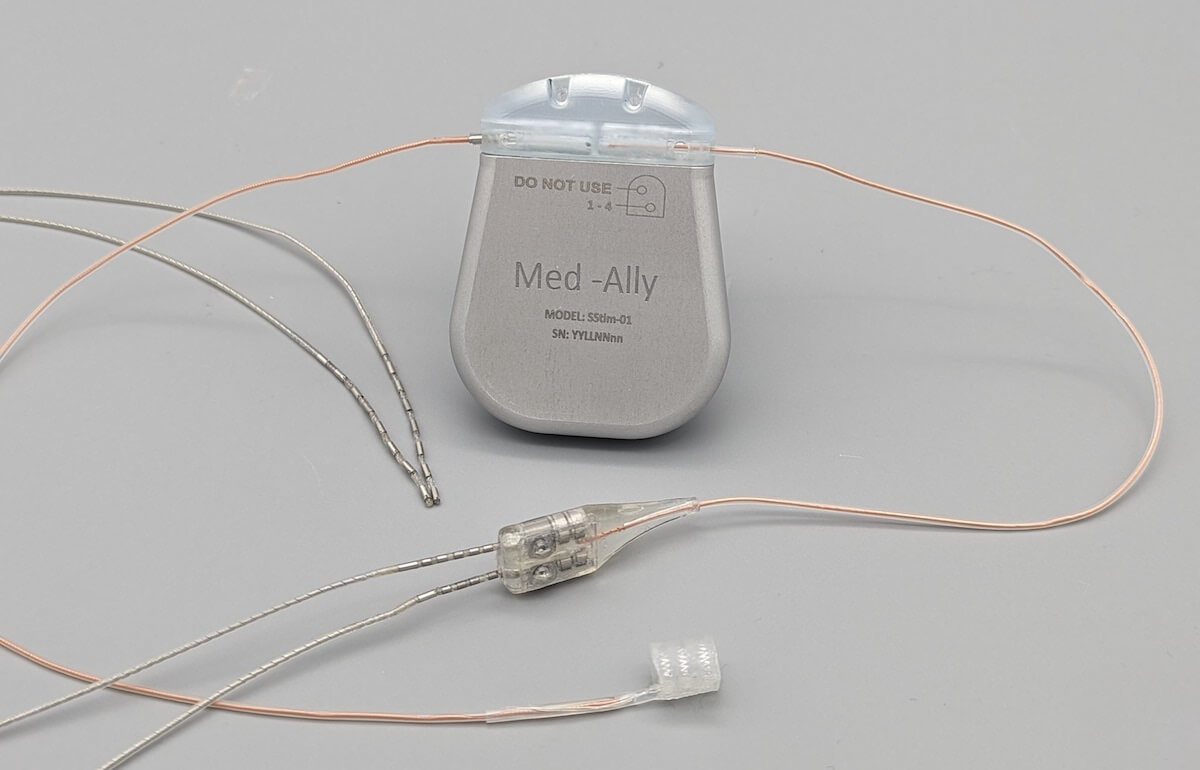
The OpenNerve Implantable Pulse Generator is an open-source medical device developed by USC’s Center for Autonomic Nerve Recording and Stimulation Systems (CARSS). Image/CARSS
From operating systems and large language models to programming languages and smartphone software, the open-source ethos has revolutionized technology, allowing coders to innovate and collaborate without being held back by licensing red-tape. A team of USC Viterbi researchers wants to know — can the same open-source approach disrupt healthcare?
Shelly and Ofer Nemirovsky Chair in Convergent Bioscience Ellis Meng leads USC’s $11.5 million NIH-funded center for open-source implantable technology, which is already empowering researchers with access to open source technology for medical device projects that target and treat the peripheral nervous system — the crucial bridge between our central nervous system and our limbs and organs.
A research team from Meng’s lab has recently conducted a wide-ranging review of the current state of play in the open-source medical device sector – examining how this approach can transform healthcare by opening collaboration pathways for medical device development, while lowering costs and expanding access to medical devices for patients. Research associate Alex Baldwin was lead author on the review, which was published in IEEE Transactions on Biomedical Engineering.
While open-source tools have become the backbone of much of today’s digital infrastructure, their adoption in MedTech has been slower and far more complex.

Shelly and Ofer Nemirovsky Chair in Convergent Bioscience and Professor of Biomedical Engineering and Electrical and Computer Engineering Ellis Meng
The medical device industry operates under stringent regulatory frameworks designed to ensure safety and efficacy. These regulations, while essential, create high barriers for entry and innovation. In the research team’s analysis, the liability associated with potential device malfunctions makes traditional manufacturers wary of open-source solutions.
Creating an open-source framework for medical devices is not as simple as the framework used by software developers, who can easily share lines of codes for other innovators to build upon.
“In order to really replicate a medical device, you need more than just code or a schematic drawing,” Baldwin said. “Quality systems, regulatory filings, and manufacturing procedures are also vital parts of the device’s source files. Documents need to have not only the testing results, but also the testing procedure very well documented,” Baldwin said.
To navigate these challenges, Baldwin and his co-authors examined a broad range of existing open-source medical device projects— case studies ranging from academic prototypes to FDA-cleared clinical tools. The review revealed a growing ecosystem, with many encouraging success stories — open-source medical device projects that are flourishing with strong community engagement and clear documentation.
“I wanted to highlight that developing a medical device as open source had been successfully done and has helped patients. Many past successes have been lower-risk devices, but I hope that this framework can expand to the more advanced devices we’re making as well and enable open-source to become more accepted and more understood by the medical device community as a whole,” Baldwin said.
The potential advantages for healthcare are many, added Baldwin. Researchers can access documented and tested devices and modify them for early laboratory studies all the way through to clinical applications.
“Currently, if a researcher wants to use an established device from a larger company in a clinical trial, they’re usually very restricted in what modifications can be made,” Baldwin said. “The company doesn’t want to do anything that could potentially compromise patient safety, which is a very good thing, but that also limits what new therapies can be developed. So, if there’s an open-source option, that broadens the field of the novel things that can be tried by researchers.”
Regulatory hurdles are still significant for researchers, but Meng noted that the emerging open-source device community was also rallying to help colleagues work around these challenges. This includes opening access to the confidential documentation that companies must send to the FDA but are normally not available to independent device developers.
“Some of those documents are now being published and shared. And so now people have a model to work from, which is hugely beneficial to anyone who’s trying to get in that space and try and avoid pitfalls,” Meng said. “This is still early days, but what’s exciting is that there could eventually be a faster road for some of these devices to actually help patients.”
The paper noted examples of successful open-source projects have shown what is possible when committed communities rally around shared needs.

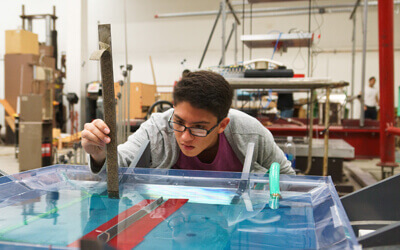
Research associate in the Alfred E. Mann Department of Biomedical Engineering Alex Baldwin.
“The Glia Project is one group that I really like. They’re doing simple things like open-source stethoscopes, open-source tourniquets and open-source otoscopes,” Baldwin said. “They found a lot of success in both Gaza and in Ukraine, in being able to just take the design, send them over there with the manufacturing methods, and they can rapidly produce, create and deploy these validated resources to people that really need them most. Importantly, these devices can be manufactured and modified in these conflict areas by local engineers and technicians, which helps build local resilience.”
In addition to reviewing the current state of the open-source device community, the research team also offers a roadmap of best practices for sustaining projects, emphasizing the need for robust documentation, transparent development processes, and partnerships with clinical users. Meng said that when her team entered the open-source space with the NIH-funded center, they did not know what other projects were out there. The lack of a comprehensive review of the open-source device sector prompted Baldwin and the team to conduct the study.
“This is like if someone has given you a book where they’ve given you a bunch of sample problems as to how to solve something,” Meng said. “From that, it’s a lot easier to take that example and then build. So, we’ve given people full insight into a system that then serves as an educational resource that otherwise just doesn’t exist. I think that’s kind of exciting.”
Meng and Baldwin noted that one of the most valuable aspects of their research into the breadth of the open-source device community was the invaluable cross-disciplinary connections made and the breaking down of the traditional silos of research.
With organizations such as OSHWA (Open-Source Hardware Association) offering leadership and connecting new medical device developers with the broader research community, the future is looking brighter for open-source MedTech, opening the doors to innovation that could reshape healthcare.
“Alex dug a lot of this stuff up and he has made a lot of connections which have already come back to benefit us,” Meng said. “We’re all just building the plane as we’re trying to fly it.”
Published on June 24th, 2025
Last updated on June 24th, 2025