Maryam Shanechi is the principal investigator on the grant (PHOTO CREDIT: Maryam Shanechi)
USC Viterbi writers follow a basic script when interviewing faculty about their work. One question we’re always told to ask is “what are the next steps for your research?” We want to end on a positive note that tells the reader what they might expect down the line. When the interview is finished, we pack it all together in a fun and informative story (like this one!) that leaves readers excited about our brave technological future.
Here, I’ll give you an example:
Just two months ago, Maryam Shanechi, the Andrew and Erna Viterbi Early Career Chair in electrical and computer engineering, said this in an article about her groundbreaking work on treating neurological and mental disorders when I asked her what the next steps were:
“We hope to build closed-loop brain-machine interfaces that adjust the dose of electrical stimulation therapy by tracking the symptoms in real-time based on brain activity and by predicting how a change in stimulation can change the activity and thus these symptoms.”
At the time, Shanechi had just shown how to predict what effect different electrical stimulation patterns and doses would have on brain activity. That work, published in Nature Biomedical Engineering, represented an important step towards personalized deep brain stimulation to address a host of neurological and mental disorders.
Now, there is already major news to report on that next step. Shanechi is the recipient and principal investigator of a $3 million grant from the National Institute of Health (NIH). The five-year project will help fund her research into that closed-loop system she mentioned as her next steps. She will collaborate with co-investigators Edward Chang, professor of neurological surgery at UCSF, and Katherine Scangos, assistant professor of psychiatry at UCSF, to test the system.
“We can finally have some real-time feedback from the brain itself and better understand how changes in electrical stimulation are directly affecting a patient’s mood symptom levels. Based on this we can give them the optimal dose of stimulation therapy at each time.” – Maryam Shanechi
Now, you may be wondering what a closed-loop system is and why it is so important to mental health? Let’s use another one of our writers’ techniques to answer that – the invaluable analogy. Think of an open-loop system as a one-way conversation. I text you the following message: “What did you think of my article about Maryam Shanechi’s research?” I wait to hear back but you ghost me. Now I’m questioning the quality of the article and my worth as a human being. Not very encouraging!
A closed-loop system is a two-way, face-to-face conversation. This time, when I ask you about the article, your eyes light up, you smile and say, “It was as entertaining as it was informative – with this $3 million NIH grant she is one step closer to helping millions of patients who are unresponsive to current treatment!”
The open-loop approach is how stimulation has so far been delivered in mental disorders; a fixed preset level of stimulation is applied and kept on at the same level over time. Now, Shanechi intends to develop a closed-loop system that personalizes and adjusts the stimulation over time by listening to the brain and how it responds to stimulation.
“With a closed-loop system we can finally have some feedback from the brain itself in real-time and better understand how changes in electrical stimulation are directly affecting a patient’s mood symptom levels. Based on this we can give them the optimal dose of stimulation therapy at each time,” Shanechi said.
The implications of Shanechi’s work and her ability to develop a closed-loop system cannot be understated. Neurological and mental disorders such as depression, addiction, and chronic pain take a huge toll on individuals and society. Our current treatment options, while they have come a long way, don’t go nearly far enough. Medication can often be expensive, addictive, or imprecise. In fact, about thirty percent of major depression patients don’t respond to any medication or psychotherapy whatsoever.
“I’m grateful to the NIH and the National Institute of Mental Health for their generous support in funding this research,” Shanechi said. “By prototyping this new neurotechnology, we can provide a proof-of-concept demonstration of the benefits of a closed-loop personalized approach to therapy, which can one day transform how we treat patients with refractory mental disorders.”
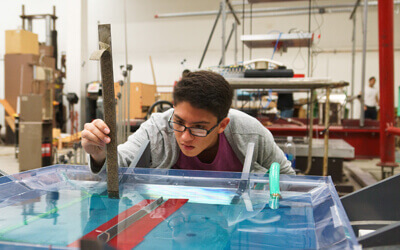
Shanechi will begin this step by working with epilepsy patients who already have intracranial electrodes implanted in their brain for standard clinical monitoring unrelated to her study (with their permission and consent, of course). While the patients are undergoing brain monitoring for their epilepsy treatment, Shanechi’s team can safely test the closed-loop system without having to do any new invasive procedures.
So, here we are at the end of another article and you should know by now how these end…with the researcher sharing their next steps. I’ll let Shanechi herself take it away:
“Now that we have the NIH funding, our next step is to start actually building and testing our closed-loop prototype neurotechnology. This would represent the first closed-loop personalized system for mental disorders that will use new machine learning models of brain response to personalize the stimulation therapy in real-time based on an individual patient’s mood symptom variations.”
Published on April 8th, 2021
Last updated on May 15th, 2025