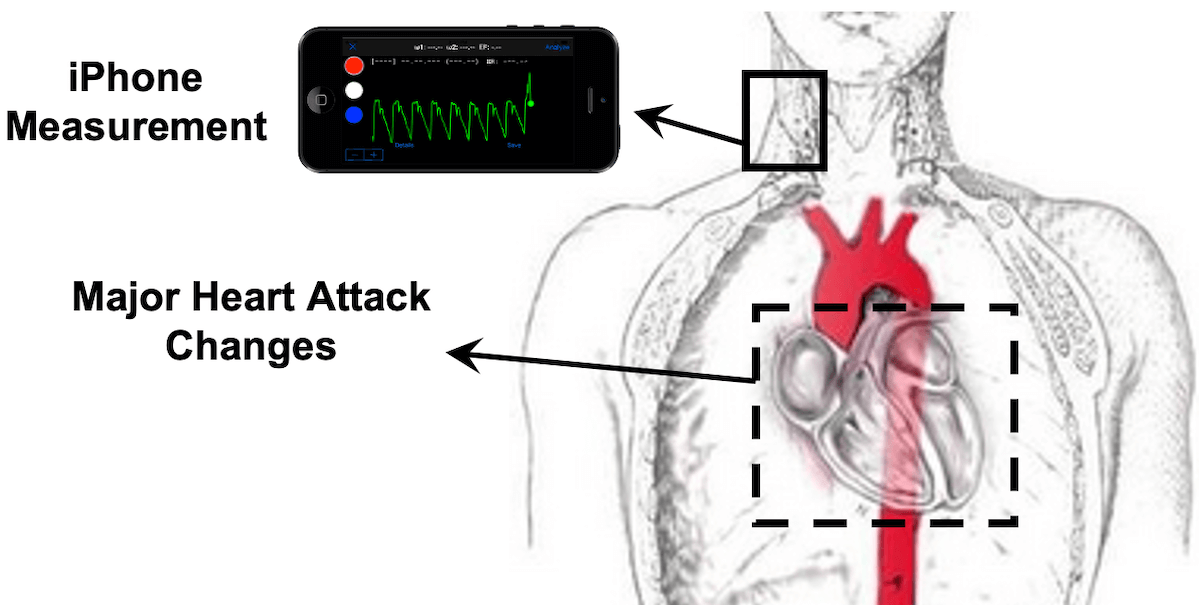
Illustration by Rashid Alavi of device design to notify patients of super-silent heart attacks
“Heart attacks are one of the leading causes of death worldwide and each year, an estimated 8.5 million cases of an acute heart attack happen worldwide, with high mortality rates of up to 10% after a month and 25% after a year,” says Rashid Alavi the lead author of a paper published in the European Society of Cardiology. However, heart attacks may not present with chest pain or in ways that people are accustomed to seeing them in the media.
More stats frame the risks: The first hour of a heart attack (myocardial infarction) represents a critical window for reducing mortality and improving patient survival (1). Heart attack is traditionally detected based on clinical symptoms such as chest pain and electrocardiogram criteria. Silent heart attacks (heart attacks with no chest pain) constitute nearly 50% of all heart attacks and are more common among diabetics and the elderly (2, 3). Furthermore, nearly half of these patients present with non-diagnostic electrocardiograms (4), referred to as “super silent” heart attacks.
It’s why Alavi, who was a doctoral student in mechanical engineering at USC within the Medical Flow Physics Laboratory (MFPL) at USC Michelson Center for Convergent Bioscience, was motivated to address the problem. Says Alavi, the earlier heart muscle is treated, the better the chance of survival. What if a non-invasive device could help provide immediate, critical warnings to those at-risk?
A new patent-pending methodology developed by the lab, directed by Professor Niema Pahlevan, the Gordon S. Marshall Early Career Chair in Engineering and Assistant Professor of Aerospace and Mechanical Engineering, and Medicine at USC, provides an alternative to existing diagnostic tools that require either expensive medical equipment like an electrocardiogram, implanted devices or blood tests for proteins released during a cardiovascular event, such as a heart attack. The researchers have created an “instantaneous, inexpensive, and non-invasive method” to detect heart attacks independently from chest pain or electrocardiograms.
The methodology the engineers have developed in collaboration with clinicians Robert Kloner, Wengde Dai, and Ray Matthews from the Huntington Medical Research Institutes and the Keck School of Medicine of USC, allows a smartphone camera or wearable device to detect a heart attack (silent, super silent, or regular) from what’s known as the neck pulse or “the pressure waveform in the carotid artery that causes the skin on the neck to pulse.”
Professor Pahlevan summarizes the technology, “We use novel physics-based metrics (or hemodynamic signatures) extracted from pressure waveforms, so our method relies on changes in mechanical activities of the heart after a heart attack.” He adds, this technology is “independent of the heart’s electrical activities.” Rather, it relies on a customized algorithm that interprets the hemodynamic data, predicting if a heart attack has occurred. “Hospitals and medical centers have excelled in minimizing the time from a heart attack patient’s arrival at the hospital to the treatment of the patients with stents or balloons that open heart vessels”, said Pahlevan. He added, “Unfortunately, heart attack patients often spend more time at home contemplating their symptoms, which exceeds the time from the hospital’s door to the crucial life-saving treatment.”
While this study was a preclinical test with animal subjects and demonstrated successful validation of the team’s novel AI-based technique, the researchers hope to start a clinical trial phase. This step is intended to translate this technology for use by clinicians and medical professionals, and, hopefully, eventually by everyone at home. Alavi, now an alumnus, continues the work as a James Boswell Postdoctoral Fellow at Caltech
1. Cannon CP, Gibson C, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283(22):2941-7.
2. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603.
3. Zhang Z-M, Rautaharju PM, Prineas RJ, Rodriguez CJ, Loehr L, Rosamond WD, et al. Race and sex differences in the incidence and prognostic significance of silent myocardial infarction in the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2016:CIRCULATIONAHA. 115.021177.
4. McCain FH, Kline EM, Gilson JS. A clinical study of 281 autopsy reports on patients with myocardial infarction. American Heart Journal. 1950;39(2):263-72.
Published on April 7th, 2024
Last updated on April 9th, 2024