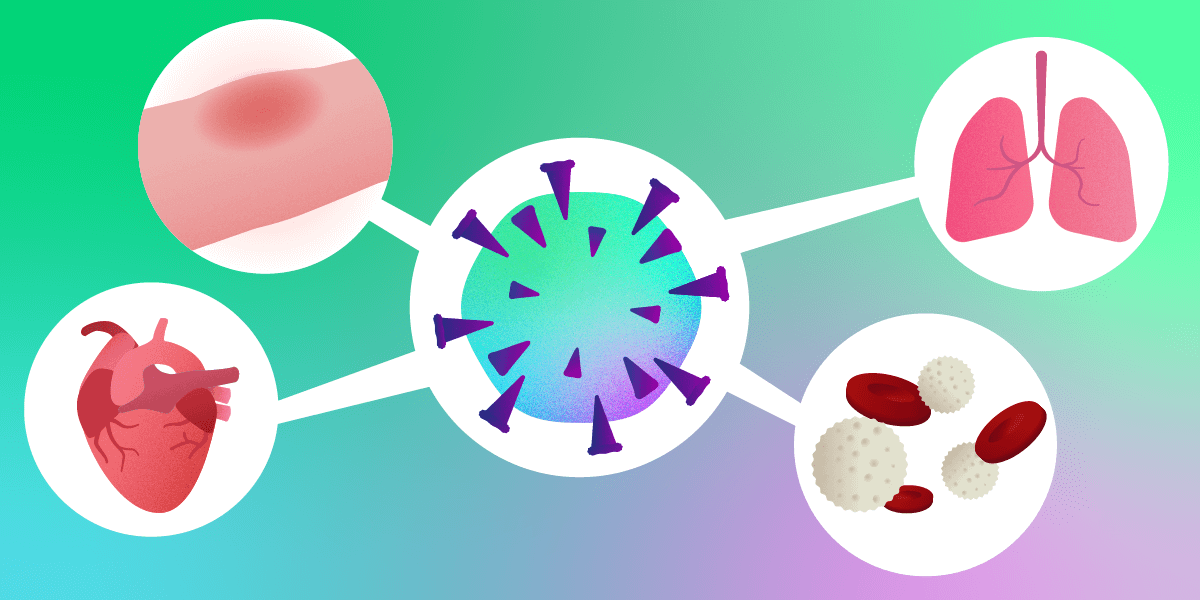
USC researchers created an algorithm that uses five data inputs to predict a patient’s COVID-19 prognosis. The features demonstrate health of the respiratory system, vascular system, immune response and inflammatory response at the time of patient intake. IMAGE/ MADELIN LUM.
Since last January 2020, much of the global pandemic has felt unpredictable, from how the healthcare system will be impacted, to how individual patients will fare with the disease. The volatile ups and downs in trying to predict these factors have created a lot of confusion, exhaustion and chaos, but what if there was an easier, earlier way to understand a patient’s prognosis?
Researchers from the USC Viterbi School of Engineering and Keck School of Medicine of USC have developed an AI algorithm that can predict a patient’s likelihood of ending up in the ICU based on five indicators taken upon initial hospitalization. The team includes Assad Oberai, Hughes Professor in the Department of Aerospace and Mechanical Engineering and his students Dhruv Patel and Vikram Kher; Neha Nanda, medical director of infection prevention and antimicrobial stewardship at Keck Medicine of USC and Infectious Disease Service-Chief, Keck School of Medicine of USC; and Vinay Duddalwar, Professor of Radiology and Director of the USC Radiomics Laboratory at the Keck School of Medicine of USC.
Multiple members from the Department of Radiology at Keck School of Medicine contributed to the study, including Steven Cen, Bhushan Desai , Ali Gholamrezanezhad and Bino Varghese. A team of research coordinators, helmed by Melissa Perkins, led data collection and repository. The research was published in Scientific Reports.
Upon intake of COVID-19 patients, medical professionals collect and record different categories of data to get a snapshot in time of the patient’s illness. The researchers used 80 pieces of medical and socio-demographic data each for over 200 patients from three Los Angeles area hospitals as inputs in algorithms to determine whether or not a patient would end up in the ICU. Once these algorithm models showed a high enough accuracy rate in predicting what actually occurred with the historic data set, the group honed in further to see how efficient they could make their model.
Oberai, who is also the vice dean for research at USC Viterbi, said: “We said, okay, out of these 80 inputs what are the pieces that the algorithm thinks are the most important? What are the five most important pieces of data? And if we work only with those, will we get similar accuracy or not? And what we found was that there were five features that gave comparable accuracy.”
The biomarkers provided information about the following medical concerns: respiratory distress (breathing rate and blood oxygen level of patient); immune response (likelihood of sepsis); circulatory system (likelihood of blood clots); and inflammation.
“What this told us,” Oberai said, “was that here is a disease that isn’t affecting just one system in the body, but is affecting many systems. Many things are going wrong at the same time, and by focusing on these five features, you can get a picture of how the disease is progressing.”
This is key in adoption of such a model, Nanda said. In her work as an infectious disease physician-epidemiologist she said few tools exist that can help you understand a patient’s prognosis in real time. Having a model that can be used “bedside” could help generate a proactive approach to patient care as it relates to criteria for admission to an intensive care unit, she said.
“Up until two weeks ago, we had zero percent ICU capacity,” Nanda said. “And so it made a lot of sense to come up with some kind of framework that would inform key stakeholders, such as clinicians, public health officials, and also healthcare administrators, to help understand resource utilization and capacity at different points in the pandemic.”
Added Duddalwar: “This sort of algorithm allows us to develop clinical workflows and predict what’s going to happen in a measurable way and prepare for demands on the healthcare system . Thanks to Assad’s work, this is done with very minimal data, using widely measured clinical features and lab metrics. The algorithms will keep learning, evolving and improving as we add more nuances and analyze effects of specific therapeutic interventions.”
It was important for the team to focus not just on creating such a model, but making it easy to use and widely applicable.
“These are all things that are easily available,” Nanda said. “We have not included any biomarkers you cannot order and will not have access to in a timely manner. All results come back within a few hours.”
The study benefited from the diversity of patients in the Los Angeles area—an element the team hopes to dive further into in next phases. But the researchers said you don’t have to be in the Western world to use their model.
Said Nanda: “The lab markers we’ve identified are available in the developing world. Everyone—whether they are in Pakistan or Bangladesh—can use these in evaluating COVID-19 patients. So I think the applicability is very wide once there has been more validation of the data.”
A Moving Target
As we’ve seen with COVID-19 in particular—and with viruses like the flu in general—the disease evolves over time. Recently, we have seen this with the COVID-19 variant B 1.1.7.
“It’s not the same disease as when we ran our study,” Oberai said. “With the variants and with therapeutics evolving, we have to ask if our models are still valid and appropriate. We also have to ask, ‘Do we want to predict the same thing as we did when the pandemic had just begun?”
In the next phase, he predicts they will go back to the algorithms and train them in a different way. “What we really want to do is keep moving the window captured by our model with the disease, retaining what is useful and leaving behind what is no longer relevant,” Oberai said.
Future of Patient Care and Management
The researchers’ work was inspired by COVID-19 and by the lack of resources often reported by hospitals over the last year, particularly in smaller hospitals with fewer ICU spots and less flexibility in managing surges. But COVID-19 isn’t the only use the team sees for such a model.
Nanda said, “In the world of infectious disease, we rarely have bedside tools we can use in discussions of prognosis. Here, one is trying to introduce a concept of that and perhaps with time, this proactive approach is something we can adopt universally to all emerging infectious diseases.
Published on March 1st, 2021
Last updated on March 1st, 2021