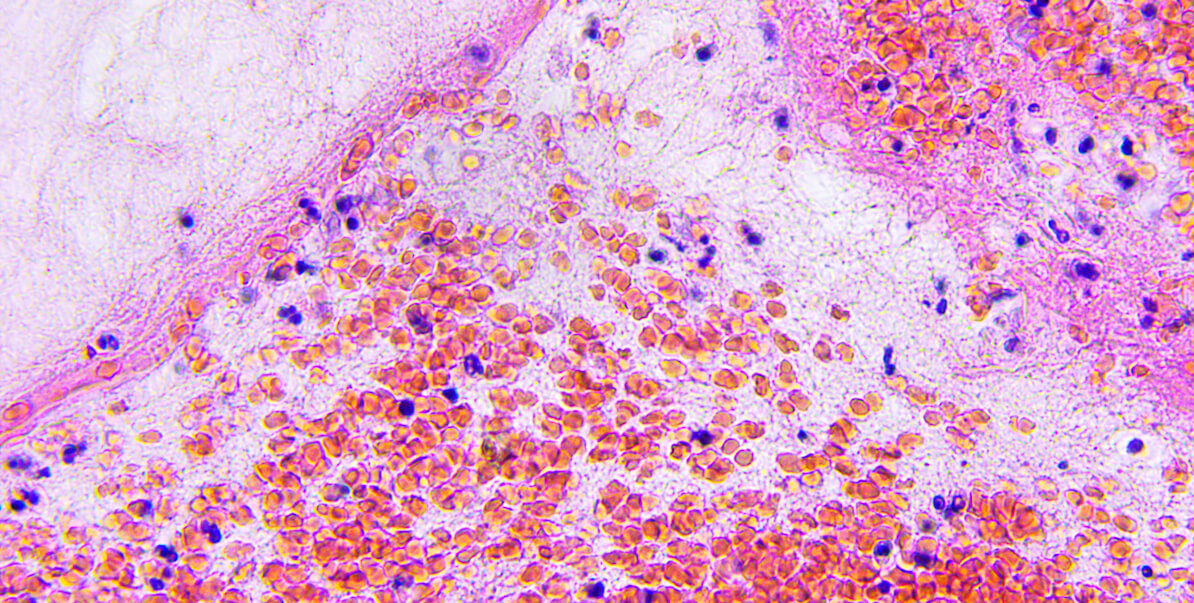
Brain tissue/ Photo credit: iStock
Researchers at USC Viterbi have designed a new drug cocktail that kills some types of brain and soft tissue cancers by tricking the cancer cells to behave as if they were starving for their favorite food–glucose. The researchers’ findings were recently published in the Journal of Biological Chemistry and may pave the way for targeted cancer treatments with greater efficacy and less harmful side effects.
To design their lethal drug combination, James H. Joly, Alireza Delfarah, Philip S. Phung, Sydney Parrish and Nicholas A. Graham in the Mork Family Department of Chemical Engineering and Materials Science first studied how cell lines from glioblastoma (brain cancer) and sarcoma (soft tissue cancer) respond to glucose starvation. They noticed that cell lines that died following glucose starvation showed a toxic buildup of the amino acid L-cystine. This led the USC team to discover that L-cystine import was causing accumulation of reactive oxygen species, highly toxic molecules that can damage cells. When the team blocked L-cystine import with drugs targeting its transporter, a protein called xCT, the cancer cells survived glucose deprivation.
Theoretically, this indicates that tumors with high xCT levels should die when starved of glucose. However, in a patient, starving cancer cells is not practical because it would mean starving their hosts (human beings). The USC researchers thus sought to kill these glucose- addicted cancer cells by designing a drug combination that mimicked the starvation-induced state. By simultaneously inhibiting a glucose transporter and an enzyme that metabolizes L-cystine, the authors found that they could set into motion metabolic processes imitating glucose deprivation, thereby forcing the cancer cells to die–even when glucose is present.
Current treatments for glioblastoma and sarcoma have limited efficacy due to acquired resistance, in which the cancer relapses by acquiring drug resistance. The use of drug combinations is thought to reduce the incidence of acquired resistance and might result in prolonged remission. In addition, the new combination of drugs might have fewer side effects since the drugs individually should have low toxicity towards non-cancerous cells. This differs from traditional chemotherapies that indiscriminately target rapidly growing cells, which results in death of many non-cancerous cells and causes side effects such as hair loss and nausea.
Moving forward, the USC Viterbi engineers are planning to partner with medical researchers from the Keck School of Medicine at USC to test this combination therapy in patient samples and mouse models of glioblastoma.
Published on February 20th, 2020
Last updated on December 7th, 2021