 Over 2000 individuals suffer from acute liver failure (ALF) each year. But ALF or acute rejection is also difficult to detect early within ICU patients who have had liver transplantation— as ultrasounds, which would normally detect a change in the stiffness of the liver (an indicator of disease or infection)— require someone to be standing by a patient continuously wielding a hand-held transducer device.
Over 2000 individuals suffer from acute liver failure (ALF) each year. But ALF or acute rejection is also difficult to detect early within ICU patients who have had liver transplantation— as ultrasounds, which would normally detect a change in the stiffness of the liver (an indicator of disease or infection)— require someone to be standing by a patient continuously wielding a hand-held transducer device.
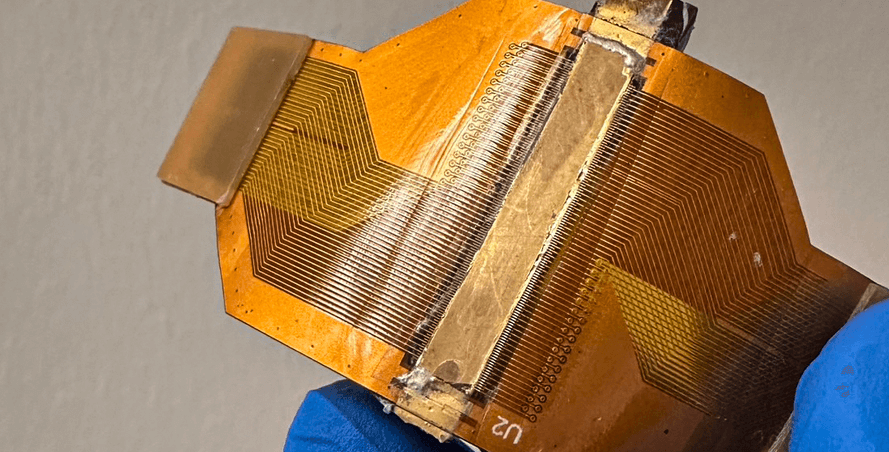
Now researchers from the USC Viterbi School of Engineering, Keck School of Medicine at USC, and the Department of Mechanical Engineering at MIT, have developed a unique adhesive “wearable ultrasound” shear wave elastography, known as BAUS-E. The scholars at USC incorporated a bioadhesive hydrogel fabricated by MIT researchers in order to adhere to the skin a wearable ultrasound device for ongoing monitoring of the liver stiffness changes for a period of two days (48 hours). The wearable ultrasound device developed by USC and MIT researchers was able to identify liver stiffnesses within six hours of its onset—a timeframe that if applied to post-operative liver transplant recipients, could allow a window of opportunity for doctors to attend to a patient’s deteriorating condition. Their paper was published in Science Advances and it is believed to be the first wearable ultrasound device that can perform ultrasound shear wave elastography with longitudinal measurements in organs.
Armed with over 40 years of institutional knowledge, the USC team was led by Research Assistant Professor Hsiao-Chuan Liu and Zohrab A. Kaprielian Fellow in Engineering and Professor of Biomedical Engineering and Ophthalmology Qifa Zhou, along with PhD students Yushun Zeng and Chen Gong. The MIT team was led by Professor Xuanhe Zhao’s group. Their miniaturized wearable ultrasound device was designed with 128 channels, comparable to those used in commercial ultrasound probes.
With this bioadhesive gel developed by MIT, the ultrasound was able to adhere to the body of a specimen for over two days. This timeframe is significant say the researchers – in particular for liver transplant patients for whom the first 72 hours after transplantation is most critical and the window in which complications are most likely to occur. Up to now, without continuous ultrasound, doctors have had to rely on taking constant biopsies or blood tests, which are more invasive. This new wearable ultrasound elastography allows for a prognosis, say the researchers, regarding the thickness and stiffness of the liver. The other advantage of this new wearable device is that it has the ability to produce acoustic radiation force impulse (ARFI) to induce shear waves, which is not normally achievable by such a small device.
The device may also help address liver failure for other at-risk patients, such as those with hepatitis, drug toxicity, or heart disease.
Method:
The researchers first had to miniaturize the wearable ultrasound technology to fit an animal model. The researchers were able to create a 24 mm long device that has 128 channels, compared to the commercial device, which has a 40 mm size. As with commercial ultrasound, the proposed wearable ultrasound can produce an acoustic radiation force impulse (ARFI) to perform shear wave elastography. This collaborative team developed miniaturized devices connected to the skin with a bioadhesive hydrogel to evaluate the stiffness changes of the organ in an animal model longitudinally.
Hsiao-Chuan Liu, the paper’s lead author, said, “The innovation is beyond the current physical wearable ultrasound device, including its small size, the ability to produce acoustic radiation forces impulse (ARFI) to produce shear waves, the ability to detect particle displacements to calculate shear velocity and the ability to continuously evaluate the stiffness changes in deep organs demonstrated in animal models.”
The next step for the research team is to try to start clinical studies for human patients.
Published on February 15th, 2024
Last updated on February 15th, 2024