The MADLab uses sewing, embroidery and lasers to create sensors and wearables. Image/Greta Harrison.
USC Viterbi’s Laboratory for the Design of Medical and Analytical Devices (MAD Lab) may seem a world away from the high-end fashion houses of Milan. But the whirl of a bobbin and buzz of a sewing machine provides a similar soundtrack.
WiSE Gabilan Assistant Professor of Biomedical Engineering Maral Mousavi and her team are exploring out-of-the-box thinking to create accessible custom sensors for affordable medical diagnostics and environmental monitoring.
The research team recently acquired a Husqvarna Viking Designer Ruby 90 deluxe sewing and embroidery machine — a software-enabled machine used in fashion settings for complex embroidering and monogramming applications. The team is adapting the technology to create custom flexible sensors for wearables and other purposes.
Mousavi’s lab creates sensors that aim to reduce the cost and inefficiency of medical testing and monitoring, making it more accessible for patients with chronic diseases and those who don’t have easy access to hospitals.

WiSE Gabilan Assistant Professor of Biomedical Engineering Maral Mousavi Maral Mousavi leads the Laboratory for the Design of Medical and Analytical Devices.
Mousavi said that traditional medical testing has a lot of inefficiencies. Patients must make multiple trips to a hospital or lab, along with follow-up appointments with the physician to discuss results and treatment options. It’s a process that doesn’t work well for patients with chronic illnesses requiring regular daily monitoring.
“We’re trying to solve this problem by changing how the analysis is performed by bringing the analysis to your home at the point of care by creating simple and accessible sensors that are worn on the body for continuous monitoring,” Mousavi said.
To do this, the lab has harnessed innovative and ubiquitous materials like yarn, thread, paper, and even nail polish to create cheap and easy-to-scale sensors.
The new Viking sewing and embroidery machine will enable the team to prototype soft and flexible wearables using custom embroidery techniques with conductive threads to create inbuilt sensors. The sensors can measure a range of health and disease biomarkers in human body fluids — such as sweat, saliva or blood.
“We detect a wide range of markers. These may be disease biomarkers that, if they’re present, they’re indicative of chronic or acute disease, or metabolites that will give information about your health,” Mousavi said. “They may also detect the medications that you need to take for a specific disease diagnosis and tell you if the dosage of the medication you’re receiving is enough to be effective.”
Melissa Banks, a Ph.D. student in the MAD Lab, regularly works with the new sewing machine. It helps that she has known her way around sewing machines since she was a seven-year-old, helping with alterations and household jobs.
“I honestly never thought my interest in textiles, sewing, and embroidery would cross over into my work with medical devices, but now that it has, it’s been a really natural transition,” Banks said. “Rigid wiring is fine for heavy equipment, but if a device is intended as a “wearable” it should be able to be worn as any other piece of clothing, and that requires knowledge of both biomedical engineering principles and textile manipulation.”

Melissa Banks, Ph.D. student in the Alfred E. Mann Department of Biomedical Engineering. Image/Melissa Banks.
Banks said the advantage of harnessing sewing and embroidery in the MAD Lab’s sensor design was the capacity the format offered for customization.
“Wearable technology may be relatively new, but clothing makers have always been problem solvers. While biomedical engineers have been optimizing methods of detection and diagnosis, textile makers have been working to optimize fit and wearability, which greatly improves the sensitivity of wearable devices,” Banks said. “With this technology, we are building on their work to make unobtrusive, custom sensors with a precise fit that feel as if they are simply part of the design.”
The Husqvarna machine allows the team to use conductive threads and fabrics created by materials scientists to form electrode patterns in infinite designs, with the machine’s software allowing intricate control of the shape and size of the electrode.
“I think the most exciting part of this work is that it makes electrochemistry a lot more approachable,” Banks said. “Rather than walking in and seeing a bench top filled with wires and electrodes, you see thread and a t-shirt. I hope that once people see what we’re doing, they might want to try their hand at designing a circuit and will fall in love with it as much as I have.”
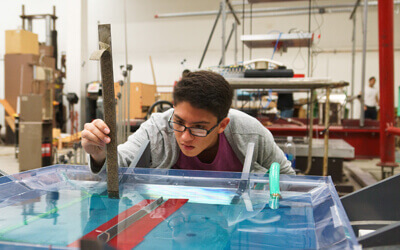
The lab also uses a CO2 laser engraver to create electrochemical sensors out of affordable polymer films. Mousavi’s team harnesses the laser to create a burn pattern of conductive carbon in a simple polymer sheet, which is then able to conduct electric signals. Mousavi said the process is environmentally friendly, as it doesn’t require the destructive chemicals or solvents usually used for processing and masking electrodes. The process is also much cheaper – where traditionally manufactured electrodes would cost around $7 each, the MAD Lab can quickly manufacture multiple electrodes on a single piece of polymer film at a cost of pennies per electrode.
“It’s very fast. This sheet of polymer costs only $1 and we can prototype a wide range of sensors with this, with a lot of flexibility for patterning and going after different designs,” Mousavi said.

Laser-engraved sensors created in the MAD Lab. Image/Abdulraham Alshami and Victor Ong.
Mousavi said the resulting sensors have applications that can target anything from soil and plant health to medical monitoring.
“For example, bipolar disorder patients have to take lithium. The medication works very well, but it has a very narrow therapeutic window — this is the concentration window in which it is going to be effective. If you go above that, it will become toxic and will cause side effects,” Mousavi said.
Mousavi said that lithium had a high risk of complications because patients have different genetic profiles and levels of water consumption, making the necessary drug intake difficult to control depending on the individual. Such complications include permanent neurological and renal damage for the patient.
“Our sensors enable a very simple at-home screening tool that you can use to frequently monitor lithium levels in different biofluids to detect an unsafe dose early.”
The MAD Lab is pioneering a range of innovative diagnostic devices as part of USC’s $11.7 million center for open-source implantables for the nervous system. Mousavi was also recently awarded a $2.3 million NIH New Innovator Award to create biocompatible nanosensors for imaging in biological media.
Find out more about the Laboratory for the Design of Medical and Analytical Devices.
Published on November 20th, 2023
Last updated on November 28th, 2023