For the millions of Americans living with traumatic brain injuries or disorders such as dementia and Alzheimer’s disease, a severe breakdown occurs in the brain’s hippocampus, the curved section of the brain that forms these episodic memories. As such, patients may have no problem recalling the distant past stored in their long-term memory. Yet, they may struggle to remember a conversation they’ve just had. Episodic memory is critical for human day-to-day life, and the loss of this ability can be devastating.
A major collaborative research project between USC Viterbi School of Engineering and Keck School of Medicine of USC is on an ambitious quest to rebuild the broken hippocampus and make episodic memory loss a thing of the past, with the help of implantable brain prostheses and a powerful predictive mathematical model.
Over 6.9 million Americans are currently living with Alzheimer’s disease and other dementias, costing the U.S. economy an estimated $360 billion in 2024, according to the Alzheimer’s Association. For these patients, their hippocampal region has been damaged beyond repair in a way that can’t benefit from traditional neuromodulation – the electrical stimulation that often treats patients with disorders such as Parkinson’s and epilepsy.

Dong Song, associate professor in USC’s Department of Neurological Surgery and the Alfred E. Mann Department of Biomedical Engineering.
Unlocking the mysteries of the brain’s hippocampus to restore lost memory has been a career-long holy grail for Dong Song, an associate professor in the Department of Neurological Surgery and the Alfred E. Mann Department of Biomedical Engineering. Song completed his Ph.D. in the USC laboratory of David Packard Chair in Engineering Ted Berger, where researchers have been working for over two decades on increasing our understanding of how the brain’s memory function works and how prostheses and algorithms can be harnessed to stimulate the hippocampal region.
Song has taken on the torch, leading his own Neural Modeling and Interface Lab at USC Viterbi, focusing on creating devices that mimic and restore cognitive function. Over the last decade, Song’s lab has worked closely with Charles Liu, the USC Neurorestoration Center director at Keck School of Medicine.
Their goal: To bring this revolutionary technology directly to the patients who desperately need it.
Liu, who has a long track record in the clinical applications of implantable brain interfaces for epilepsy patients, said that his interest was immediately piqued when he first heard about Berger and Song’s memory restoration research.
“The first thing I thought of was, ‘How can we take this into humans?'” Liu asked. “The excitement gets substantially higher, and the stakes are higher when you can get the device into humans. Of course, you need a device that passes regulatory approval. Nothing’s real until you get to that point. Finally, you must come up with a concept that is commercially sustainable.”
The team faced some seemingly insurmountable logistical hurdles. How could they jump through the stringent regulatory hoops required for human trials while accessing patients willing to have these devices implanted into their brains?
Luckily, Liu and his colleagues at the USC Epilepsy Care Consortium work closely with groups of epilepsy patients who were already being treated for their seizures with FDA-approved brain-computer-interface implants. The patients were also dealing with episodic memory loss related to their epilepsy. So, it seemed fortuitous that Song’s computational models could harness their existing implants to stimulate their brains, mimicking the hippocampal episodic memory connection.
“By piggybacking on devices that are already there, we would minimize the risk of future development to address the second problem these patients have, which is a memory problem,” Liu said.
“Dong, the team, and I all looked at each other and said, ‘You know, this will actually work,'” Liu added.
How the brain interface works to improve memory
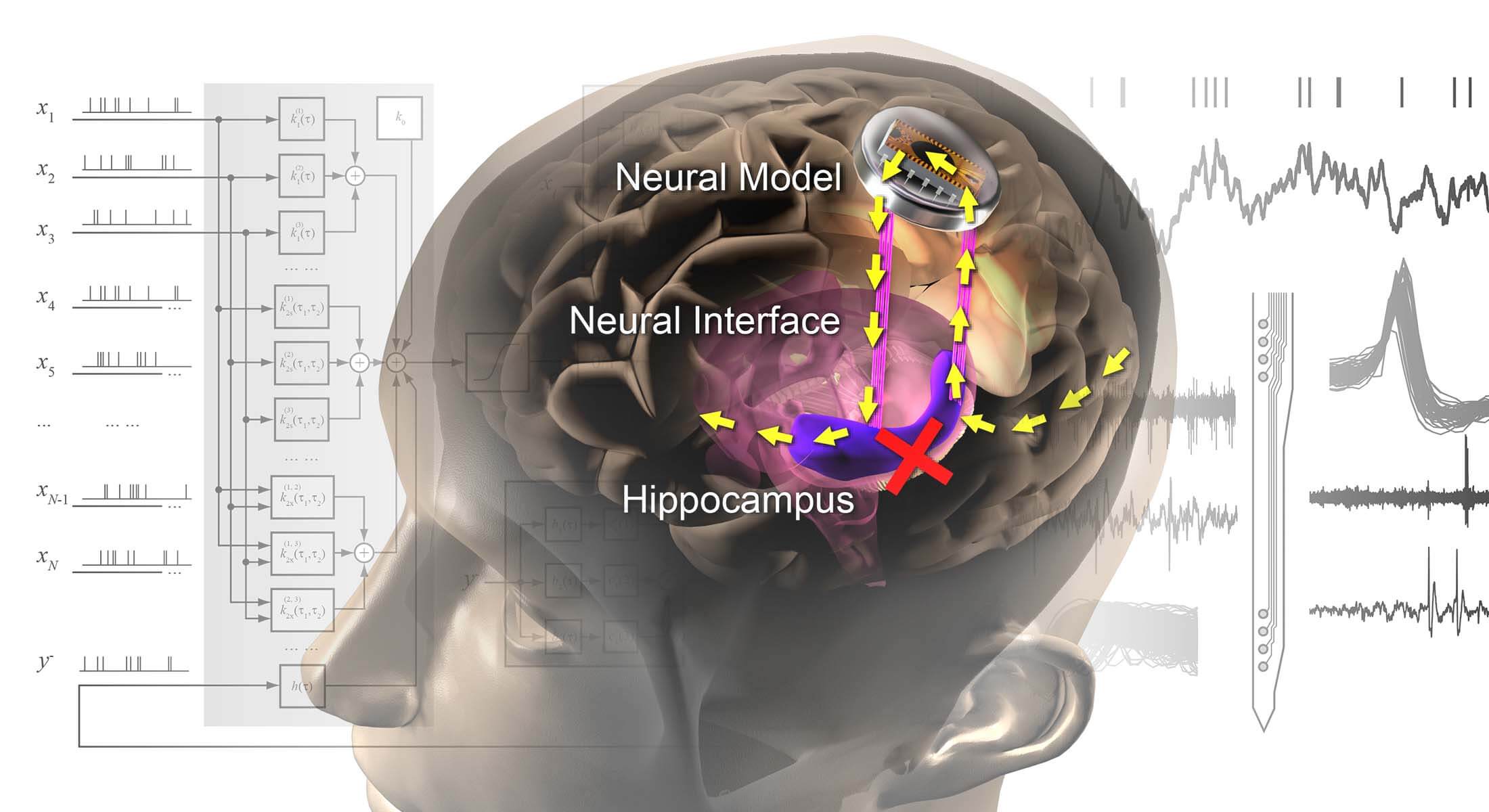
The prosthesis being developed by the USC Viterbi and Keck School of Medicine team replaces the connection that has been broken in a damaged hippocampus, restoring lost memories. Image/USC Neural Modeling and Interface Lab.
Song describes the brain interface system as effectively rebuilding a broken bridge in the hippocampus. The device works by recording information from the upstream region of the patient’s brain and then, via cable, feeding that information into external hardware housing Song’s computational model, which has been built from vast amounts of brain data to mimic the natural signaling behavior of the brain.
“[We are] using a computational model to predict the correct signal for the hippocampus and stimulating that pattern back to the hippocampal downstream region,” Song said. “By doing that, it is almost like you’re fixing the broken bridge. You restore the signal transmission from the upstream region to the downstream region, and by doing that, hopefully, you restore the function.”
“We are not writing any false information into the brain,” Song said. “We just take what is already in the pipeline, but it’s broken somehow. We fix that broken part, and it flows again. The memory is all the patient’s own memory.”
Promising human trials show enhanced memory function
Charles Liu, USC Neurorestoration Center director at Keck School of Medicine.
The team worked with a group of 24 epilepsy patient volunteers between 2016 and 2021. As part of their standard of care, the epilepsy patients had already undergone surgical implantation of electrodes in their brains. For Liu, this was an important factor, as the patients were not required to take on any additional risk by taking part in the memory study. The patients were stationed in an epilepsy monitoring unit for upwards of a week while the electrodes monitored the occurrences of their seizures. It provided the researchers with plenty of time to concurrently run their memory testing. The patients worked with Song, Liu, and their graduate students on a series of tasks to determine the effect of the stimulation on their memories.
“These patients would have electrodes placed in the hippocampus, and we would target specific subfields of the hippocampus as relevant to Dong’s computational models,” Liu said.
“As they’re performing these memory tasks, the single unit recordings are captured, and then Dong takes these and runs them through his computational model. And then, based on the simulations, he’d apply the stimulation back through the electrodes to enhance their memory,” he added.
Song said that the patients were shown sets of images and were then asked to recall these images at different intervals — seconds after the test, as well as days later. Song said that because the hippocampus was not a sensory area, the participants reported that they did not feel the low level of stimulation they received through the tests. The experiment also used control trials where participants received no stimulation or randomized stimulation.
“What we found, in short, is when we applied stimulation according to the computational model, we can enhance the memory function, meaning the percentage of the times patients make a correct choice of the image is higher in our test group than in the other two controls,” Song said.
The team discovered that volunteers using the memory prosthesis displayed an 11% to 54% improvement on the memory tests. Song and Liu said that the results were an exciting first step on the path towards clinical application of the technology.
“When I first watched Dong and the graduate students actually performing the tasks in our human patients in the epilepsy unit, that was a hugely important proof of concept that this particular group of patients can actually participate in the treatment of a problem that they have,” Liu said.
Added Song: “We definitely have a lot of work to do. But I feel like we have a pathway to begin to do this work.”
An exciting future full of memories for patients with brain disorders
USC is a research breeding ground for brain-computer interfaces that could change the game for Alzheimer’s, dementia and brain injury patients. New treatments for conditions affecting the brain or other parts of our nervous system are enabled by the availability of cutting-edge research tools. Song has been working with Professor Ellis Meng, the Shelly and Ofer Nemirovsky Chair in Convergent Biosciences, on a major BRAIN Initiative project to create high-tech, super-thin polymer brain implants and distribute them to the research community. The resulting resource center — the Polymer Implantable Electrode (PIE) Foundry — has provided over 1000 microfabricated neural interfaces to neuroscience and neural engineering researchers worldwide in the last five years.

Ellis Meng, Shelly and Ofer Nemirovsky Chair in Convergent Biosciences.
“The PIE Foundry is like a 3D printing shop for neural interfaces where researchers can rapidly prototype complete microelectrode devices at USC and receive plug-and-play tools for their labs,” Meng said.
“Ellis Meng is an expert in the MEMS (micro-electromechanical systems) technology,” Song said. “You need to make these devices really small so that there’s not too much tissue damage to the brain. Secondly, it needs to be soft because brain tissue doesn’t like rigid things — it treats them as a foreign object. That’s basically what Ellis and I have been working on for many years: developing polymer-based flexible miniaturized devices for recording and stimulation in the brain. With this more advanced interface technology, we can potentially handle more complex memories.”
USC is also home to a National Institutes of Health-funded center for developing open-source implantable systems for simulating and recording from the autonomic nervous system, led by Meng. These interfaces are designed and manufactured at USC in Meng’s Biomedical Microsystems Lab and the John O’Brien Nanofabrication Lab.
For Song, Liu and their team, the long-term goal is to develop their work into a fully implantable miniaturized polymer electrode device that can implement the computational models and record and stimulate the hippocampus without the need for an external cable and hardware setup. They plan to initiate new human studies within the next 1-2 years, utilizing more advanced neural interface and modeling technologies that are being developed now. This phase will go beyond proof-of-concept, aiming to develop a device that is closer to clinical applications.
Again, close collaboration between Keck School of Medicine and USC Viterbi is key to the success of this brain and memory research. Song said that without the direct pipeline to patients that Liu and Keck School of Medicine offered, his team’s research would remain stuck in the lab.
“Only with Charles could we have access to test the prosthetic in humans,” Song said.
“I’m convinced that the things that we can’t do will be possible through engineering,” Liu added. “It’s how human beings have always solved problems. I tell Dong all the time: ‘In the end, you guys are all working on solving the problems that we and our patients have.’ I think that’s really exciting.”
Published on October 30th, 2024
Last updated on October 30th, 2024